Yes, Lasix (furosemide) is a potent diuretic that significantly reduces sodium levels in the body. This occurs because Lasix inhibits sodium and chloride reabsorption in the loop of Henle, leading to increased excretion of both sodium and water in urine.
The extent of sodium depletion depends on several factors including the dose of Lasix administered, the patient’s overall health, and other medications they are taking. Higher doses naturally lead to greater sodium loss. Patients with pre-existing conditions like heart failure or kidney disease might experience more pronounced sodium depletion. Always consult with your doctor or pharmacist to understand the potential impact on your specific situation.
Monitoring sodium levels through regular blood tests is crucial, especially for individuals on long-term Lasix therapy. Symptoms of significant sodium depletion, known as hyponatremia, include muscle weakness, fatigue, nausea, and confusion. If you experience any of these, contact your healthcare provider immediately. Early detection and management are key to preventing serious complications.
Remember: This information is for educational purposes and does not constitute medical advice. Always discuss medication management with your doctor before making any changes to your treatment plan. They can provide personalized guidance based on your individual needs and health history.
- Does Lasix Deplete Sodium?
- Lasix’s Mechanism of Action: How it Affects Sodium
- NKCC2 Inhibition: The Key to Sodium Depletion
- Other Factors Influencing Sodium Levels
- Sodium Levels Before, During, and After Lasix Treatment
- Symptoms of Sodium Depletion Caused by Lasix
- Risk Factors for Severe Sodium Depletion with Lasix
- Lasix Dosage and its Impact on Sodium Levels
- Monitoring Sodium Levels During Lasix Therapy
- Interpreting Sodium Levels
- Dietary Strategies to Manage Sodium Levels While on Lasix
- Sodium Content in Common Foods
- Potassium-Rich Foods
- Alternative Diuretics and Their Sodium-Depleting Effects
Does Lasix Deplete Sodium?
Yes, Lasix (furosemide) is a potent diuretic that significantly depletes sodium. It works by inhibiting sodium and chloride reabsorption in the loop of Henle, leading to increased excretion of both sodium and water in urine.
This sodium loss can be substantial, potentially causing hyponatremia (low blood sodium levels) if not carefully monitored. Symptoms of hyponatremia include nausea, vomiting, confusion, and muscle weakness. In severe cases, it can be life-threatening.
Regular blood tests are recommended to monitor sodium levels, particularly during initial treatment and any dosage adjustments. Your doctor will likely advise you on appropriate dietary sodium intake to minimize the risk of depletion. This often includes adjusting your salt intake to compensate for the sodium loss caused by Lasix.
Important Note: Never alter your Lasix dosage without consulting your physician. They can adjust the medication and monitor your sodium levels to prevent complications.
Other factors influencing sodium depletion include pre-existing conditions, other medications, and individual responses to Lasix. Open communication with your healthcare provider is key for safe and effective Lasix treatment.
Lasix’s Mechanism of Action: How it Affects Sodium
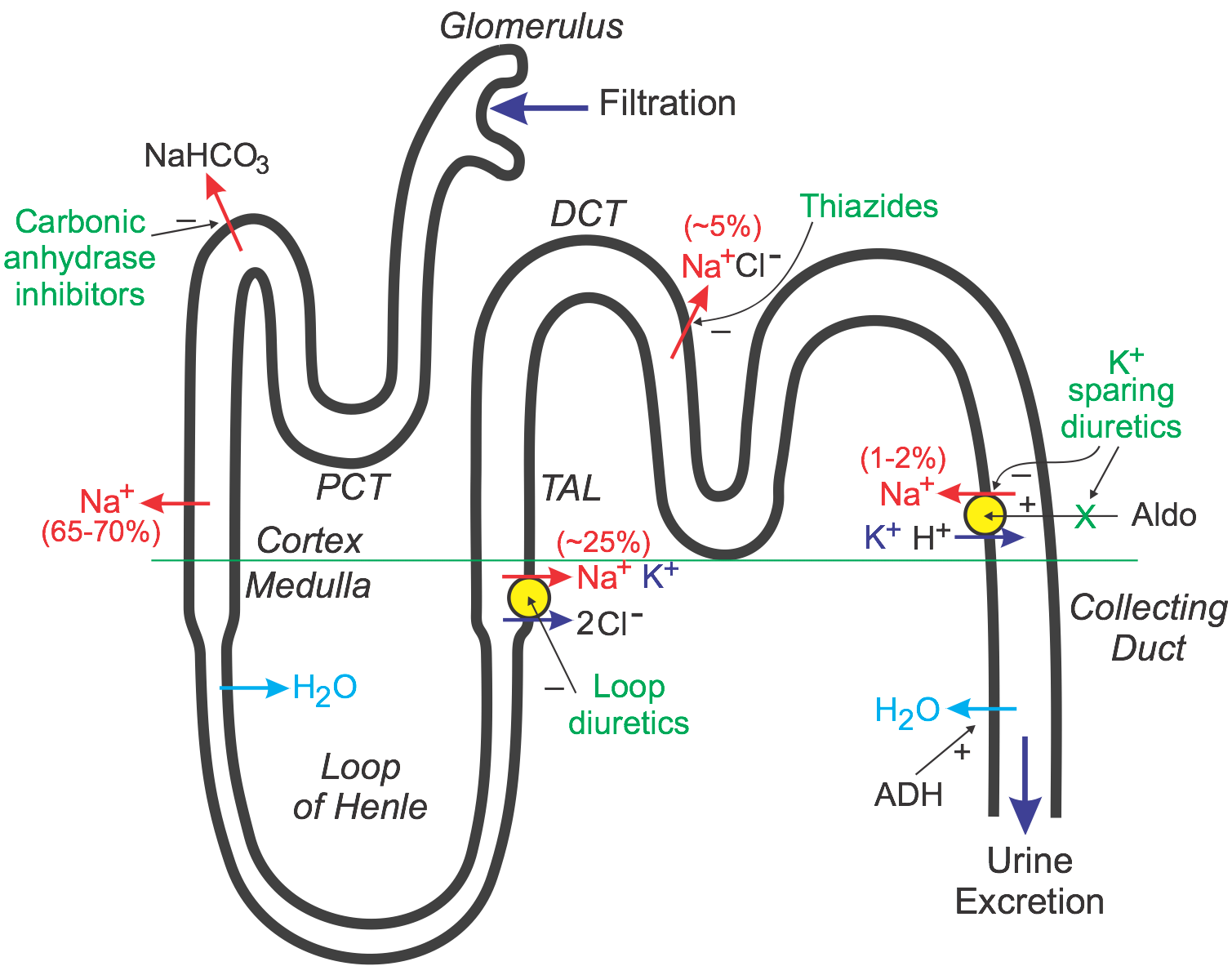
Lasix, or furosemide, powerfully increases sodium excretion by directly inhibiting the sodium-potassium-chloride cotransporter (NKCC2) in the thick ascending limb of the loop of Henle.
NKCC2 Inhibition: The Key to Sodium Depletion
This inhibition prevents the reabsorption of sodium, potassium, and chloride ions back into the bloodstream. Consequently, a larger amount of these electrolytes is passed into the urine, leading to increased urination (diuresis) and a decrease in blood volume.
- Reduced sodium reabsorption directly leads to lower sodium levels in the blood (hyponatremia).
- This effect is significant, making Lasix a potent diuretic frequently used to treat conditions involving fluid retention.
Other Factors Influencing Sodium Levels
While NKCC2 inhibition is the primary mechanism, other factors influence the extent of sodium depletion.
- Dose: Higher doses of Lasix lead to greater sodium excretion.
- Individual factors: Patient’s kidney function, overall health, and other medications affect the response.
- Dietary sodium intake: High sodium intake can partially offset Lasix’s effects, while low sodium diets enhance it.
Regular monitoring of serum sodium levels is crucial when using Lasix, especially in patients at risk for electrolyte imbalances.
Sodium Levels Before, During, and After Lasix Treatment
Monitoring sodium levels is key when using Lasix. Your doctor will likely order blood tests before starting Lasix to establish your baseline sodium level.
During Lasix treatment, expect a decrease in sodium levels. The extent of the decrease depends on several factors, including your dosage, overall health, and other medications you are taking. Regular blood tests help your doctor manage your treatment and adjust your dosage as needed to prevent excessive sodium depletion.
After you stop Lasix, your sodium levels usually return to normal. However, the recovery rate varies individually. Your doctor will continue to monitor your sodium levels to ensure they are stabilizing and within a healthy range. They might schedule follow-up blood tests to confirm this.
| Stage | Sodium Level Expectations | Recommendations |
|---|---|---|
| Before Lasix | Baseline measurement establishes your starting point. | Follow your doctor’s instructions for pre-treatment blood work. |
| During Lasix | Expect a decrease; frequency of monitoring depends on your condition and dosage. | Report any symptoms of low sodium (e.g., weakness, dizziness) immediately. Maintain adequate fluid intake unless otherwise advised. |
| After Lasix | Gradual return to normal levels; monitoring continues to ensure stability. | Attend all scheduled follow-up appointments and blood tests. |
Close communication with your healthcare provider is vital for safe and effective Lasix treatment. Never adjust your medication dosage without consulting your doctor.
Symptoms of Sodium Depletion Caused by Lasix
Lasix, a powerful diuretic, can lead to low sodium levels (hyponatremia) if not carefully managed. Recognizing the signs is crucial for timely intervention.
Mild symptoms may include:
- Muscle weakness or cramps
- Headache
- Nausea
- Lethargy
- Slight confusion
More severe symptoms demand immediate medical attention and can involve:
- Severe muscle weakness or paralysis
- Seizures
- Loss of consciousness
- Severe vomiting
- Significant changes in mental status, such as disorientation or hallucinations
If you experience any of these symptoms while taking Lasix, contact your doctor immediately. Your doctor can monitor your sodium levels through blood tests. They may adjust your Lasix dosage or prescribe supplemental sodium to correct the imbalance.
Prevention is key. Maintain a balanced diet rich in sodium, especially if prescribed Lasix for extended periods. Your physician will provide personalized guidelines.
This information is for educational purposes only and does not constitute medical advice. Always consult with your healthcare provider for any health concerns or before making any decisions related to your health or treatment.
Risk Factors for Severe Sodium Depletion with Lasix
Patients with pre-existing low sodium levels (hyponatremia) face a significantly higher risk of severe depletion when taking Lasix. Regular monitoring of sodium levels is critical for these individuals.
Kidney disease, particularly those with impaired renal function, increases the susceptibility to severe sodium loss. This is because the kidneys play a crucial role in sodium regulation.
Liver cirrhosis disrupts the body’s sodium balance, making patients more vulnerable to severe depletion with Lasix. Close monitoring and adjusted dosing are often required.
Heart failure, particularly in advanced stages, can predispose patients to severe sodium depletion. The combination of Lasix and underlying heart issues requires careful medical supervision.
Diuretic use in combination with other medications that promote sodium excretion amplifies the risk of depletion. This includes some other diuretics and certain antihypertensive drugs.
Older adults, due to age-related physiological changes, experience a heightened risk of severe sodium loss. Their response to Lasix may be different, necessitating careful dose adjustments.
Dehydration exacerbates the effects of Lasix, leading to a faster and more severe drop in sodium levels. Maintaining adequate hydration is paramount.
Individuals with a history of severe sodium depletion are at significantly increased risk of recurrence with Lasix. These patients need close observation and potential adjustments to their treatment plan.
Vomiting or diarrhea, which causes fluid and electrolyte loss, increases the risk of severe sodium depletion in conjunction with Lasix. Managing underlying gastrointestinal issues is important.
Lasix Dosage and its Impact on Sodium Levels
Lasix’s effect on sodium levels directly correlates with its dosage. Higher doses generally lead to greater sodium excretion. A typical starting dose for edema is 20-80 mg, but this can vary significantly based on individual needs and response.
For example, a patient with severe edema might require a much higher dose, perhaps 80-160 mg, initially, leading to substantial sodium loss. Conversely, lower doses, like 20-40 mg, may produce a more modest reduction in sodium levels. Regular monitoring of sodium levels is crucial to ensure the dose remains appropriate and prevent dangerous depletion.
Always consult a physician before adjusting Lasix dosage. Inadequate monitoring can result in hyponatremia, a condition of dangerously low sodium levels. Symptoms include nausea, vomiting, confusion, and even seizures. Careful titration of the dose, guided by regular blood tests, is key to minimizing this risk.
Factors influencing sodium depletion beyond dosage include kidney function, diet, and the presence of other medical conditions. Patients with impaired kidney function, for instance, may experience amplified sodium loss at lower Lasix doses. Dietary sodium intake also plays a role; a high-sodium diet might partially offset the diuretic effect.
Regular blood tests provide vital information about sodium levels. These results, along with the patient’s overall response to Lasix, allow physicians to fine-tune the dosage. Close collaboration with a healthcare professional is vital for safe and effective Lasix use.
Monitoring Sodium Levels During Lasix Therapy
Regularly monitor serum sodium levels. Aim for blood tests at least weekly, especially during initial therapy adjustments. More frequent monitoring might be necessary for patients at higher risk of hyponatremia, such as the elderly or those with pre-existing conditions affecting fluid balance.
Interpreting Sodium Levels
Hyponatremia (low sodium) is a potential side effect. Sodium levels below 135 mEq/L warrant attention. Mild hyponatremia (130-135 mEq/L) often requires adjustments to Lasix dosage or supplementary sodium intake. Severe hyponatremia (below 130 mEq/L) necessitates immediate medical intervention. Always correlate sodium levels with clinical signs and symptoms–fatigue, confusion, nausea, and muscle weakness can indicate low sodium.
Conversely, hypernatremia (high sodium) is less common but still possible. Levels above 145 mEq/L require investigation and potential modification of the treatment plan. This might involve adjusting Lasix dosage or addressing underlying causes of dehydration.
Close collaboration between the patient, physician, and nursing staff is critical. Patients should be educated on recognizing symptoms of both low and high sodium levels and promptly reporting them to their healthcare provider. Accurate record-keeping of sodium levels and Lasix dosage is fundamental for effective management.
Dietary Strategies to Manage Sodium Levels While on Lasix
Reduce processed foods significantly. These are often high in hidden sodium. Aim for whole, unprocessed foods whenever possible.
Choose fresh fruits and vegetables. They naturally contain low sodium and offer potassium, which can help counter Lasix’s effects.
Limit canned goods. Many canned foods contain added sodium as a preservative. Opt for fresh or frozen alternatives when feasible.
Sodium Content in Common Foods
| Food | Approximate Sodium Content (mg per serving) |
|---|---|
| 1 slice white bread | 150-200 |
| 1 cup canned soup | 600-900 |
| 1 oz salted pretzels | 200-300 |
| 1 cup cooked spinach | 70-80 |
Carefully read food labels. Pay close attention to the sodium content listed per serving. Smaller portions can help manage sodium intake.
Use herbs and spices instead of salt. Experiment with different flavor profiles to enhance your meals without relying on salt.
Drink plenty of water. Adequate hydration helps your kidneys function properly and flushes out excess sodium.
Potassium-Rich Foods
Increase your intake of potassium-rich foods like bananas, sweet potatoes, and avocados. Potassium helps balance the effects of Lasix on sodium levels. However, consult your doctor before significantly increasing your potassium intake, as high potassium levels can be harmful.
Consult a registered dietitian or nutritionist. They can provide personalized guidance on creating a low-sodium meal plan tailored to your specific needs and health conditions.
Alternative Diuretics and Their Sodium-Depleting Effects
Lasix, while effective, isn’t the only diuretic option. Many alternatives exist, each with varying sodium-depleting capabilities. Choosing the right one depends on individual needs and health conditions.
Here’s a breakdown of some common alternatives and their effects:
- Thiazide Diuretics (e.g., Hydrochlorothiazide): These moderately deplete sodium, primarily acting on the distal convoluted tubule of the kidney. They are often prescribed for hypertension and are generally well-tolerated. Expect a milder sodium loss compared to Lasix.
- Potassium-Sparing Diuretics (e.g., Spironolactone, Amiloride): These minimally affect sodium levels. Their primary mechanism involves potassium retention, making them useful in conjunction with other diuretics that deplete potassium. Sodium excretion is a secondary effect.
- Loop Diuretics (other than Lasix, e.g., Bumetanide, Torsemide): These, like Lasix, powerfully deplete sodium by acting on the loop of Henle. However, their potency and side effect profiles can differ. Consult your doctor to determine which is best suited for you.
- Carbonic Anhydrase Inhibitors (e.g., Acetazolamide): These diuretics primarily act on the proximal convoluted tubule, leading to bicarbonate excretion and, to a lesser extent, sodium loss. They’re often used for specific conditions like altitude sickness and glaucoma, not generally for significant sodium depletion.
Important Note: The degree of sodium depletion varies considerably depending on dosage, individual factors (kidney function, overall health), and the interaction with other medications. Always consult your doctor or pharmacist before starting or changing any diuretic medication. They can help you select the most appropriate diuretic and dosage based on your specific health circumstances, ensuring safe and effective sodium management.
- Monitor your sodium levels: Regular blood tests can help track your sodium levels and adjust medication accordingly.
- Consider dietary changes: A diet low in sodium can complement diuretic therapy, supporting better sodium balance.
- Be aware of side effects: Each diuretic carries potential side effects. Discuss these with your doctor and report any unusual symptoms promptly.