Prednisone isn’t a first-line treatment for bronchial infections; antibiotics usually tackle the bacterial cause. However, prednisone’s anti-inflammatory properties can significantly reduce inflammation and associated symptoms like coughing and wheezing, offering relief especially during severe cases.
Your doctor might prescribe prednisone alongside antibiotics if your infection is particularly severe or if symptoms don’t respond adequately to antibiotics alone. This combined approach aims to quickly control inflammation and expedite recovery. Expect a course lasting several days to a week, depending on your individual response and the severity of your infection. Remember, always follow your doctor’s instructions meticulously regarding dosage and duration.
Side effects are possible. Common ones include increased appetite, weight gain, mood swings, and difficulty sleeping. Serious side effects are less frequent but necessitate immediate medical attention. Report any unusual symptoms to your doctor immediately. Careful monitoring, especially for those with pre-existing conditions like diabetes or hypertension, is crucial. Prednisone shouldn’t be taken without consulting a medical professional; self-medication is strongly discouraged.
This information serves as a guide and doesn’t replace professional medical advice. A thorough diagnosis by a doctor is paramount before starting any treatment for a bronchial infection. They will assess your specific situation, consider other possible causes, and determine the most appropriate treatment plan tailored to your needs. Discuss potential risks and benefits of prednisone treatment with your physician.
- Prednisone for Bronchial Infections: When is it Necessary?
- Severe Cases and Specific Situations
- Who Might Benefit?
- Cautions and Considerations
- Alternative Treatments
- Understanding Prednisone’s Role in Bronchial Infection Treatment
- How Prednisone Works
- When Prednisone is Prescribed
- Potential Benefits and Risks of Prednisone for Bronchial Infections
- Dosage, Duration, and Monitoring Prednisone Treatment for Bronchial Infections
Prednisone for Bronchial Infections: When is it Necessary?
Prednisone, a corticosteroid, isn’t a first-line treatment for most bronchial infections. Doctors generally prefer antibiotics or antiviral medications for bacterial or viral infections, respectively.
Severe Cases and Specific Situations
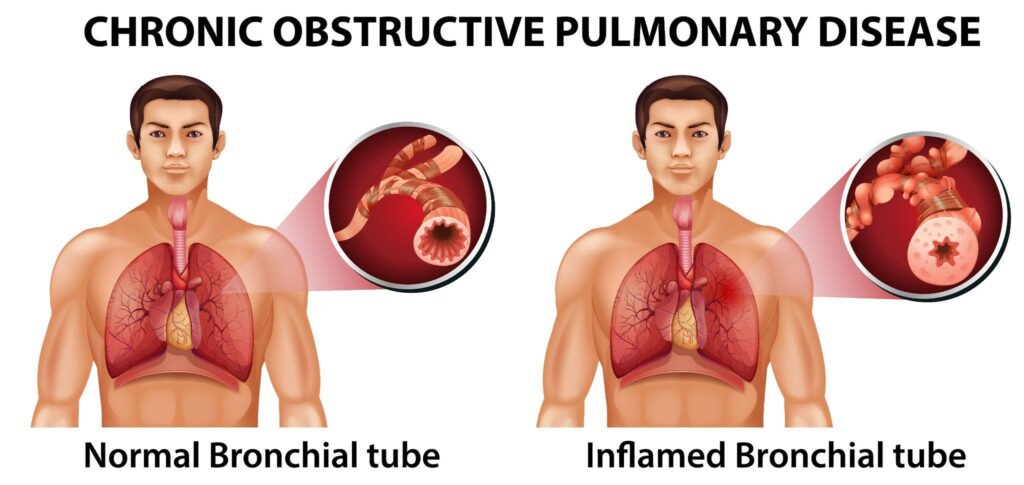
However, prednisone might be necessary in specific circumstances. Consider its use in severe cases of acute bronchitis, where significant airway inflammation causes substantial breathing difficulties. This often manifests as severe wheezing or shortness of breath that doesn’t respond to bronchodilators. Similarly, prednisone can help manage exacerbations in individuals with chronic obstructive pulmonary disease (COPD) experiencing a significant worsening of symptoms.
Who Might Benefit?
Patients with a history of asthma or other reactive airway diseases may find prednisone beneficial during a bronchial infection, particularly if they have significant airway inflammation and bronchospasm. Its anti-inflammatory properties can help reduce swelling in the airways. Always consult your doctor; they’ll assess your medical history and current symptoms to determine if prednisone is appropriate for you. Doctors consider factors such as the severity of your symptoms, your response to other treatments, and your overall health before prescribing this medication.
Cautions and Considerations
Remember: Prednisone has potential side effects, including increased blood sugar, increased risk of infections, and insomnia. Long-term use carries further risks. Therefore, it’s crucial to use prednisone only under strict medical supervision. Self-medicating is never advisable.
Alternative Treatments
Before considering prednisone, your doctor will likely explore other treatment options, such as bronchodilators (to open airways) and appropriate antibiotics or antiviral medications depending on the cause of your infection. These treatments often effectively manage bronchial infections without the need for corticosteroids.
Understanding Prednisone’s Role in Bronchial Infection Treatment
Prednisone doesn’t directly kill the bacteria or viruses causing your bronchial infection. Instead, it reduces inflammation and swelling in your airways. This helps relieve symptoms like coughing, wheezing, and shortness of breath.
How Prednisone Works
Prednisone is a corticosteroid that suppresses your immune system’s response. This reduces the inflammatory process that contributes significantly to bronchial infection symptoms. By lessening airway inflammation, you breathe easier. The medication is most helpful for managing severe symptoms. It frequently works best when combined with other therapies targeting the infection itself, such as antibiotics for bacterial infections.
When Prednisone is Prescribed
Doctors typically prescribe prednisone for severe bronchial infections causing significant breathing difficulty or when other treatments haven’t provided sufficient relief. The duration of treatment varies depending on the severity of your condition and your response to medication. Always adhere to your doctor’s instructions for dosage and duration.
Remember, prednisone is not a cure for bronchial infection. It’s a tool to manage symptoms and improve your comfort while other treatments address the underlying infection.
Potential Benefits and Risks of Prednisone for Bronchial Infections
Prednisone, a corticosteroid, isn’t a first-line treatment for most bronchial infections, but it can offer benefits in specific situations. Doctors often consider it for severe cases to reduce inflammation and improve breathing.
Potential Benefits:
- Reduced inflammation: Prednisone powerfully reduces airway swelling, easing breathing difficulties associated with severe bronchitis or other inflammatory bronchial conditions.
- Faster symptom improvement: Studies show that in some patients with severe exacerbations of COPD or asthma complicated by bronchial infection, prednisone can lead to quicker relief from coughing, wheezing, and shortness of breath.
- Improved lung function: Reduced inflammation translates to improved airflow, as measured by pulmonary function tests.
Potential Risks:
- Increased risk of infection: Prednisone weakens the immune system, potentially prolonging or worsening a current infection, or increasing susceptibility to new infections. This risk necessitates careful monitoring.
- Side effects: Common side effects include increased blood sugar, weight gain, fluid retention, mood changes, insomnia, and increased appetite. Severe side effects are possible, but less common.
- Medication interactions: Prednisone interacts with many other medications. Your doctor needs a complete medication history before prescribing it.
- Mask underlying infections: The anti-inflammatory effect of prednisone could mask symptoms of a bacterial or fungal infection, delaying appropriate treatment with antibiotics or antifungals.
- Withdrawal symptoms: Stopping prednisone abruptly can cause withdrawal symptoms. Dosage reduction must be gradual, under medical supervision.
Important Considerations:
- Prednisone is usually a short-term treatment for bronchial infections, not a long-term solution.
- The decision to use prednisone should be made on a case-by-case basis by a physician, considering the severity of the infection and the patient’s overall health.
- Regular monitoring of blood sugar and blood pressure is typically necessary during prednisone treatment.
- Always inform your doctor about all medications and supplements you are taking.
Dosage, Duration, and Monitoring Prednisone Treatment for Bronchial Infections
Prednisone dosage for bronchial infections varies greatly depending on the severity of the infection and the patient’s individual response. Your doctor will determine the appropriate dose, typically ranging from 20-60 mg daily. This may be administered as a single dose or divided into multiple doses. Lower doses are often used for milder infections.
Treatment duration usually lasts from 5 to 10 days. However, your doctor may adjust this based on your symptoms and clinical response. A shorter course is preferable to minimize side effects. Always follow your doctor’s prescribed regimen.
Regular monitoring is critical. Expect your doctor to schedule follow-up appointments to assess your progress. They’ll monitor your symptoms, check blood pressure and blood sugar levels (if applicable), and assess for potential side effects like insomnia, increased appetite, or mood changes. Report any new or worsening symptoms immediately.
Specific blood tests might be ordered to track your response and adjust treatment accordingly. Your doctor may also recommend chest X-rays or other imaging to assess the infection’s resolution.
Remember, Prednisone is a powerful medication. Never adjust your dosage or discontinue treatment without consulting your physician. Open communication with your healthcare provider is key to successful treatment and minimizing potential risks.