Reactive arthritis often resolves on its own within a year, but it can linger for much longer. Complete remission is possible for many, while others experience ongoing symptoms requiring long-term management.
Early and aggressive treatment significantly improves your chances of a quicker recovery. This includes medications to manage inflammation and pain, like NSAIDs or biologics. Physical therapy plays a crucial role in restoring joint function and preventing long-term disability. A tailored exercise plan helps rebuild strength and mobility.
Lifestyle adjustments are also key. A healthy diet, weight management (if needed), and stress reduction techniques can positively impact symptom severity and overall well-being. Regular follow-up appointments with your rheumatologist are essential to monitor progress and adapt the treatment plan as necessary. Don’t hesitate to ask questions and actively participate in your care.
While complete resolution isn’t guaranteed for everyone, proactive management offers the best chance for a positive outcome. Focus on building a strong partnership with your healthcare provider to develop a personalized strategy that meets your specific needs. Remember, managing reactive arthritis is a process, and consistent effort yields the best results.
- Does Reactive Arthritis Go Away?
- Factors Influencing Recovery
- Managing Long-Term Symptoms
- Seeking Professional Help
- Understanding Reactive Arthritis’s Course
- Typical Timeline for Symptom Resolution
- Factors Influencing Recovery Time
- Typical Symptom Resolution Stages
- Long-Term Outlook
- Factors Influencing Recovery Time
- Lifestyle Adjustments
- Individual Factors
- Treatment Adherence
- Disease Severity
- Treatment Options to Speed Recovery
- Medication
- Lifestyle Adjustments
- Other Therapies
- Important Note:
- Long-Term Management and Prevention of Recurrence
- Medication Adherence
- Lifestyle Adjustments
- Physical Therapy
- Stress Management
- Vaccination
- Early Intervention
- When to Seek Further Medical Attention
- Signs Requiring Urgent Care
- Living with Reactive Arthritis: Maintaining Quality of Life
- Managing Pain and Fatigue
- Staying Active and Connected
- Seeking Professional Support
Does Reactive Arthritis Go Away?
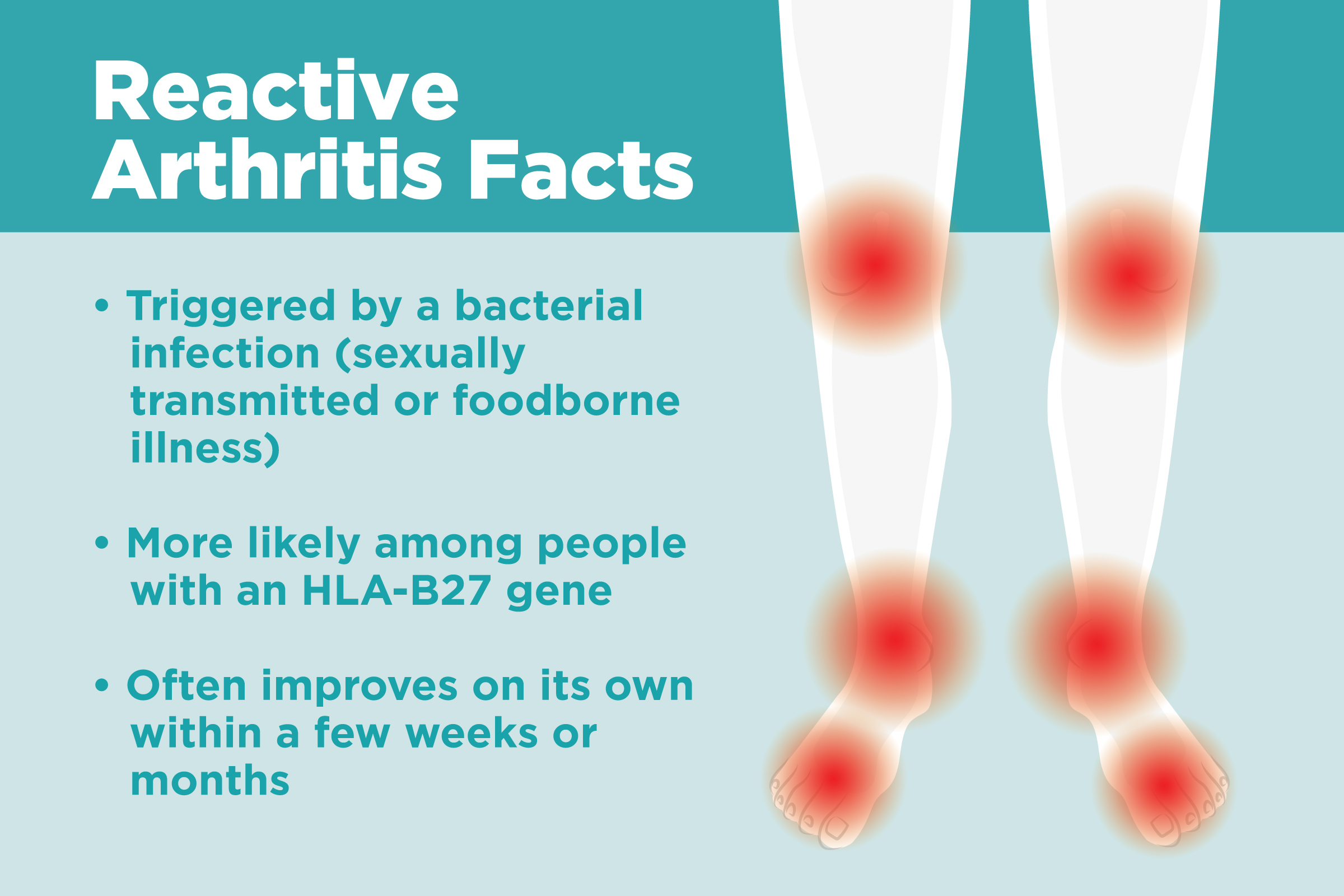
Reactive arthritis often resolves itself within a few months, with many experiencing symptom relief within a year. However, for some, symptoms can persist longer, even becoming chronic.
Factors Influencing Recovery
Several factors influence recovery time. The severity of the initial infection triggering the arthritis plays a significant role. Early diagnosis and treatment significantly improve outcomes. A prompt and aggressive treatment plan involving medication, physical therapy, and lifestyle modifications is key. Your doctor will personalize a plan tailored to your specific needs and condition.
Managing Long-Term Symptoms
While many individuals experience complete remission, some may experience ongoing symptoms, such as joint pain or stiffness. In these cases, long-term management focuses on pain control and preserving joint function. This might include ongoing medication, regular physical therapy, and adaptive strategies for daily activities.
Seeking Professional Help
Early intervention is crucial. If you suspect you have reactive arthritis, consult a rheumatologist or other healthcare professional immediately. They can diagnose the condition and create a treatment strategy to minimize long-term effects and improve your quality of life. Don’t hesitate to contact your doctor to discuss concerns or changes in your symptoms.
Understanding Reactive Arthritis’s Course
Reactive arthritis typically resolves within a few months. Most people experience significant improvement within 6-12 months, with many seeing complete remission. However, a small percentage will develop chronic symptoms lasting longer.
The severity and duration vary greatly depending on individual factors like the triggering infection and overall health. Some individuals experience only mild discomfort, while others face more intense and persistent joint pain and inflammation.
Early diagnosis and treatment are key to a faster recovery. Aggressive management, often including medication and physical therapy, helps minimize long-term complications and speeds up healing. Consistent adherence to treatment plans is crucial for optimal results.
Chronic reactive arthritis may require ongoing medical management. This may involve medication to manage pain and inflammation, as well as regular physiotherapy to maintain joint mobility and prevent disability.
While complete resolution is common, some individuals may experience flare-ups or persistent low-level symptoms. Close monitoring by a rheumatologist is recommended to ensure timely intervention during any relapses.
Lifestyle adjustments, such as maintaining a healthy weight, following a balanced diet, and engaging in regular moderate exercise, also contribute to better outcomes and improved quality of life.
Typical Timeline for Symptom Resolution
Reactive arthritis symptoms usually improve within several months. Many people see significant relief within 1-3 months of diagnosis, with most symptoms resolving completely within a year.
Factors Influencing Recovery Time
- Severity of initial infection: A more severe initial infection (like salmonella or shigella) may lead to a longer recovery period for reactive arthritis.
- Prompt treatment: Early intervention with medication, including NSAIDs and sometimes disease-modifying antirheumatic drugs (DMARDs), can shorten the course of the illness.
- Individual response to treatment: Each person’s immune system and response to therapy vary; some individuals will respond better and faster than others.
- Presence of complications: Development of complications, such as uveitis (eye inflammation), can extend recovery time.
While most people experience substantial improvement within a year, some may experience persistent symptoms, particularly joint stiffness or pain, for longer.
Typical Symptom Resolution Stages
- Weeks 1-3: Intense pain and inflammation often decrease. Mobility generally improves.
- Months 1-6: Most significant symptom improvement. Many individuals return to normal activities.
- Months 6-12: Lingering symptoms, like mild joint stiffness, may persist in some individuals but generally improve further. Follow up with your doctor remains important.
Remember, this is a general guideline. It’s crucial to consult your doctor for personalized advice based on your individual health status and response to treatment. They can help manage your symptoms and develop a long-term plan for care.
Long-Term Outlook
While reactive arthritis can be debilitating during the acute phase, the long-term prognosis is usually good. Complete remission is common, though some people experience occasional flare-ups.
Factors Influencing Recovery Time
Early diagnosis and treatment significantly shorten recovery. Prompt initiation of appropriate medication, such as NSAIDs or antibiotics if an infection is present, helps manage symptoms and reduce inflammation.
Lifestyle Adjustments
Maintaining a healthy lifestyle accelerates healing. A balanced diet rich in fruits, vegetables, and lean protein supports your immune system. Regular, moderate exercise improves overall health and reduces joint stiffness. Adequate rest and stress management are also key. Aim for 7-8 hours of sleep nightly and explore relaxation techniques like yoga or meditation to mitigate stress.
Individual Factors
Recovery time varies considerably. Factors such as the severity of the initial infection, overall health, and genetic predisposition all play a role. Younger individuals often recover faster. Pre-existing conditions like autoimmune diseases can impact recovery. Smoking and excessive alcohol consumption impede healing and should be avoided.
Treatment Adherence
Consistent adherence to the prescribed treatment plan is paramount. This includes taking medication as directed, attending all follow-up appointments, and diligently performing any recommended physical therapy. Skipping doses or neglecting appointments delays recovery.
Disease Severity
The intensity of initial symptoms directly correlates with recovery time. More severe initial presentations typically require longer treatment periods and potentially different treatment strategies. This is something you should discuss with your doctor.
Treatment Options to Speed Recovery
Managing reactive arthritis focuses on reducing inflammation and managing symptoms. This often involves a multi-pronged approach.
Medication
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen and naproxen reduce pain and swelling. Always follow prescribed dosages.
- Corticosteroids: Prednisone, a powerful anti-inflammatory, may be used for short periods to manage severe inflammation. Long-term use has side effects, so it’s usually a temporary solution.
- Disease-modifying antirheumatic drugs (DMARDs): Methotrexate and sulfasalazine can slow disease progression in some cases. Your doctor will consider these if NSAIDs and corticosteroids are insufficient.
- Biologics: These targeted medications, such as TNF inhibitors, may be prescribed for those with severe, persistent symptoms that don’t respond to other treatments. They specifically target the inflammatory process.
Lifestyle Adjustments
- Physical Therapy: Regular exercise, guided by a physical therapist, helps maintain range of motion and strength, preventing stiffness and disability. Focus on low-impact exercises.
- Occupational Therapy: This can help adapt daily tasks to manage joint pain and limitations.
- Rest: Adequate rest is crucial for your body to heal. Avoid overexertion, especially during flares.
- Diet: A balanced diet rich in anti-inflammatory foods like fruits and vegetables can support overall health. Consider reducing foods known to trigger inflammation for some individuals.
Other Therapies
- Heat and Cold Therapy: Applying heat or cold packs to affected joints can provide temporary pain relief. Experiment to find what works best for you.
- Assistive Devices: Canes, braces, or splints can provide support and reduce strain on affected joints.
Important Note:
This information is for general knowledge and does not substitute professional medical advice. Always consult your doctor or rheumatologist for a proper diagnosis and personalized treatment plan. They can help you determine the best course of action for your individual circumstances and monitor your progress.
Long-Term Management and Prevention of Recurrence
Regular checkups with your rheumatologist are key. These visits allow for early detection of flares and adjustment of your treatment plan as needed. Consistent monitoring helps maintain remission and reduces the risk of future episodes.
Medication Adherence
Strictly following your prescribed medication regimen, even during periods of remission, is crucial. Missing doses can trigger a relapse. Discuss any concerns or side effects with your doctor promptly to find solutions that work for you. Consider using a pill organizer or setting medication reminders to improve adherence.
Lifestyle Adjustments
Identifying and managing triggering factors is vital. This involves pinpointing specific infections (like those from Chlamydia trachomatis or Salmonella) or foods that exacerbate symptoms. Maintain excellent hygiene practices to minimize infection risk. A balanced diet, regular exercise (avoiding overexertion during flares), and sufficient sleep support overall health and contribute to better disease management.
Physical Therapy
Physical therapy can significantly improve joint mobility and reduce pain. A physical therapist will create a personalized exercise program to strengthen muscles, improve range of motion, and manage joint stiffness. This proactive approach helps prevent long-term disability.
Stress Management
Stress can worsen reactive arthritis symptoms. Incorporate stress-reducing techniques into your daily routine. This could include mindfulness exercises, yoga, or other relaxation methods. Learning to manage stress contributes significantly to overall well-being and disease control.
Vaccination
Stay up-to-date with vaccinations. Certain vaccines protect against infections that can trigger reactive arthritis. Discuss vaccination recommendations with your doctor.
Early Intervention
Recognize early warning signs of a flare-up, such as joint pain, swelling, or fatigue. Contact your doctor immediately if you notice any of these symptoms. Early treatment helps minimize the severity and duration of the flare.
When to Seek Further Medical Attention
Contact your doctor immediately if you experience increased joint pain or swelling, especially if it’s accompanied by fever, skin rashes, or eye inflammation. These could indicate a complication or worsening of your condition.
Signs Requiring Urgent Care
Seek immediate medical attention if you notice significant limitations in your daily activities due to joint pain, difficulty breathing, or chest pain. These symptoms might point to more serious problems requiring rapid intervention.
Also, if your prescribed medication isn’t managing your symptoms effectively, or if you experience any new or unusual symptoms, schedule a visit with your rheumatologist or doctor as soon as possible. Open communication about your concerns is key for appropriate management of reactive arthritis.
Living with Reactive Arthritis: Maintaining Quality of Life
Prioritize regular, low-impact exercise. Aim for at least 30 minutes most days of the week. Activities like swimming, cycling, or gentle yoga can help improve joint mobility and reduce stiffness. Listen to your body; stop if you experience pain.
Manage stress levels effectively. Stress exacerbates inflammation. Incorporate stress-reducing techniques into your daily routine, such as meditation, deep breathing exercises, or spending time in nature. Consider joining a support group for connection and shared experiences.
Follow a balanced diet. Reduce foods known to trigger inflammation, like processed foods, red meat, and refined sugars. Increase your intake of anti-inflammatory foods, including fruits, vegetables, and omega-3 fatty acids. Consult a registered dietitian for personalized dietary advice.
Managing Pain and Fatigue
Learn different pain management strategies. Over-the-counter pain relievers (NSAIDs) can help. Your doctor might suggest other medications or therapies, such as physical therapy. Consider alternative therapies like acupuncture or massage, but discuss these with your doctor beforehand.
Pace yourself and prioritize rest. Fatigue is a common symptom. Learn to recognize your limits and schedule rest periods throughout the day. Avoid overexertion, which can worsen symptoms.
Staying Active and Connected
Adapt your daily routines. Make necessary adjustments to your home and work environment to minimize strain on your joints. Use assistive devices as needed. Don’t hesitate to ask for help from family or friends.
Maintain social connections. Reactive arthritis can be isolating. Make an effort to stay connected with loved ones and participate in activities you enjoy. Social interaction provides emotional support and can positively influence mental well-being.
| Activity | Frequency | Benefits |
|---|---|---|
| Low-impact exercise | Daily (30 minutes) | Improved mobility, reduced stiffness |
| Stress management techniques | Daily | Reduced inflammation, improved mood |
| Balanced diet | Ongoing | Reduced inflammation, improved overall health |
| Rest and pacing | As needed | Fatigue management, symptom control |
Seeking Professional Support
Regularly consult your rheumatologist. They can monitor your condition, adjust treatment plans as needed, and provide ongoing support. Don’t hesitate to discuss any concerns or changes in your symptoms.